New Vaccines for a Novel Virus: Insights from Coronavirus and Vaccine Experts
Conversations with Arnold S. Monto and Emily Toth Martin

Arnold Monto
Thomas Francis Jr. Collegiate Professor of Public Health and Co-Director of the Michigan Influenza Center

Emily Toth Martin
Associate Professor of Epidemiology and
Co-Director of the Michigan Influenza Center
In 2017 Arnold Monto gave a plenary address at a National Institutes of Health event convened to develop a strategic research agenda for developing a universal influenza vaccine. That agenda formed the foundation of what is now the Michigan Influenza Center, one of five sites across the country that collects influenza vaccine effectiveness data for the Centers for Disease Control and Prevention.
Arnold and I co-lead the Michigan Influenza Center, and throughout the pandemic we have been conversing regularly and been interviewed by local, state, national, and international media. These excerpts of our conversations provide our insights on what we know and what we are looking for as coronavirus vaccines are administered across the nation and world.
How do these vaccines give us protection against COVID-19?
Monto. Immunity to this coronavirus seems to be related to a specific protein—the spike protein—that allows entry of the virus into cells. Fortunately, this spike protein was identified earlier in work with SARS and MERS as the important target for development of a successful coronavirus vaccine. All of the vaccines being developed—whatever the platform—are focused on the spike protein.
Three different approaches—or platforms—are used here to get the body to produce antibodies. A fourth possibility, injecting virus-like particles (VLP), is also being studied.
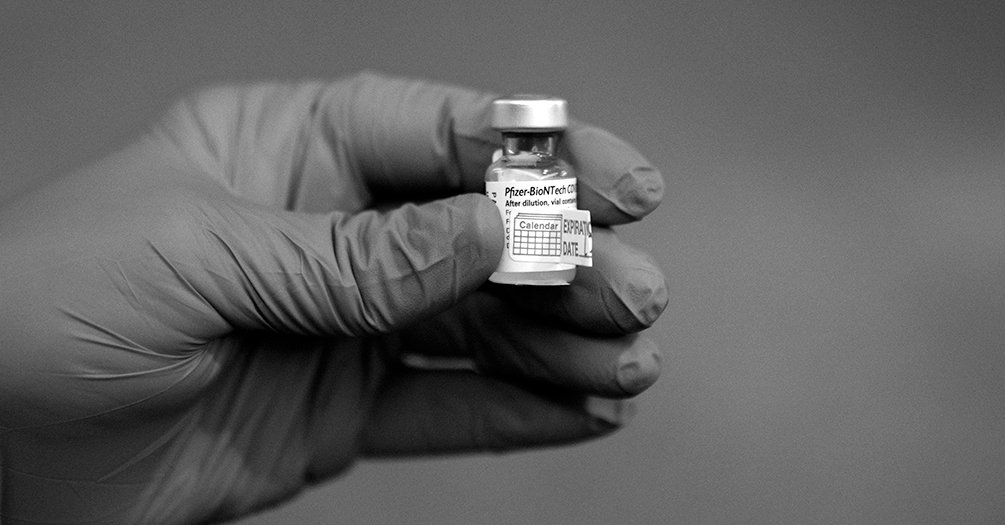
- Nucleic-Acid Vaccines. This new technique uses genetic material derived from that of circulating viruses—in this case RNA—to get the body to mimic the viral replication process. The proteins from this process initiate an immune response and the creation of antibodies to the virus. The Moderna and Pfizer-BioNTech strategy is to use mRNA—messenger RNA—as the genetic message.
- Vector Vaccines. These vaccines insert genetic material from the spike protein into an adenovirus construct, a virus that causes common colds and other illnesses in humans but has been altered so it cannot replicate. The adenovirus construct serves as a vector to deliver RNA from the coronavirus spike protein to the human immune system. To avoid human antibodies to adenoviruses from previous infections derailing the whole process, these vaccines use chimpanzee adenoviruses or uncommon human viruses as a starting point.
- Protein Vaccines. This is a more traditional approach combined with a new process. First, they use the viral genetic material to get cell cultures to develop the spike protein that will result in production of antibodies. Then, the protein is combined with an adjuvant, a substance intended to improve the immune response.
The nucleic-acid vaccines took the lead because they are easily produced. Approval of the Johnson & Johnson vaccine, using a vector platform and highly effective, gives us more options and has advantages like being a single dose and not having cold-storage challenges.
How were we able to move so quickly and create multiple successful vaccines?
Martin. For me, the federal government’s Warp Speed terminology passed over the fact that these vaccine technologies have been in development for years. I don’t think we saw a speed-versus-safety tradeoff.
Monto. Agreed. The Star Trek reference suggested the vaccines were developed with undue speed. In fact, that’s not the case. We did compress into a one-year period what typically takes up to 10 years or more. But no corners were cut when it came to safety. How are we doing it? As Dr. Martin mentioned, we worked off existing vaccine technologies, including things that were put in place to address the original SARS virus, MERS, or other coronaviruses. We telescoped some studies—doing them in parallel rather than sequentially. Operation Warp Speed coordinated units of the federal government. The National Institutes of Health harmonized efficacy trials and coordinated all networks conducting studies. In some cases, units conducting studies on other diseases were temporarily redeployed to do COVID-related work. By and large, everyone used harmonized data sets and combined safety monitoring boards looking at the studies.
Public-private partnership also made a big difference. Typically, a company would never manufacture a product before it had federal safety approval to be sold on the market. But once certain benchmarks were reached, vaccine manufacturers produced and prepared vaccines for distribution before they were approved for emergency use, knowing they might be delayed or even rejected. But with the world in need of vaccines and many funds given to the effort, this became a major success story of the response to the pandemic.
We still are doing exactly what we ordinarily do with vaccine development but on a shorter timeline. Every standard step for development of any vaccine is being followed but being done quickly and efficiently. As an example, at the start of the work, there were resources given to studies in small and then large laboratory animals for spike antibody production. This justified going into studies in humans.
In looking at the entire process, the only difference in efficacy standards between emergency use authorization and what happens in more traditional time frames is that we really can’t compress time as we study the duration of immunity. There is no indication we’ll have any surprises, but you never fully know what will happen until you actually observe it.
How do we know the vaccines are effective?
Martin. Effectiveness means several things—most importantly preventing disease in the vaccinated person and perhaps preventing transmission. Transmission has been a difficult question for years. If a vaccine prevents disease in the vaccinated person, does it also prevent them from transmitting the virus to others?
Monto. Defining effectiveness—or efficacy—is a choice we make in these processes. The FDA decided to use COVID-19 disease of any severity. They could have used preventing severe disease but settled on disease of any severity. Preventing severe disease is looked at as an important but secondary outcome.
Regulators established greater than 50% efficacy for prevention of disease of any severity as the endpoint for approval, not realizing efficacy would be as high as we are seeing. A secondary endpoint was going to be prevention of severe disease. To everyone’s pleasant surprise, we have nearly 100% prevention of serious disease for all COVID vaccines.
We’ve had to totally rethink asymptomatic transmission since this virus emerged. With the original SARS virus, there was little evidence of asymptomatic transmission. This virus seems to be more efficient at transmitting asymptomatically, predominantly so in some outbreaks.
–Arnold Monto
We’re seeing hardly anyone who is vaccinated develop severe disease. That may not continue as the most vulnerable receive vaccines. Some people with underlying conditions might still have severe disease, since nothing is ever 100%. But the numbers are encouraging.
Martin. Asymptomatic transmission has been the big puzzle. The problem in our studies is this: If you have a mild infection that is mostly or entirely asymptomatic and you are spreading the disease to some extent, it might not show up in vaccine trials, which measure who got sick. Theoretically, you could receive one of the COVID vaccines, get an asymptomatic infection that the study doesn’t register, and still be shedding a bit of virus and potentially transmitting to others. With a 95% efficacy rate, I have trouble believing this is a concern. But with how well this virus seems to spread asymptomatically, I want to wait for the data to see whether transmission is possible after vaccination.
Monto. We’ve had to totally rethink asymptomatic transmission since this virus emerged. With the original SARS virus, there was little evidence of asymptomatic transmission.
This virus seems to be more efficient at transmitting asymptomatically, predominantly so in some outbreaks. These are reasons to get the vaccine. A more vaccinated population will help us learn more about transmission. Special studies in populations, such as households, will help in determining this.
Martin. And if we have vaccines with a wide range of protection—preventing infection and transmission—that gives us tools for ongoing control of COVID-19. Once we can move past an emergency situation and can do these studies in specific populations, we’ll have a clearer picture.
How do we know the vaccines are safe?
Monto. With anything that’s new, we are very concerned about safety. Aside from the allergic reactions that very rarely produce anaphylaxis—a concern with past vaccines too—there are very few safety concerns with the approved vaccines. Even though the trials were relatively large, as you scale up distribution, you have to watch carefully for rare side effects. You might have seen that a hold was placed on a particular vaccine by the Data Safety Monitoring Board because they saw some adverse side effects. That pause in the process of developing a vaccine shows just how cautious we’ve been with monitoring and how well the system works.
The FDA established 3,000 participants as an initial minimum, and with tremendous investments put into vaccine development—including around communication and recruiting—we had large numbers of people involved in initial trials, over 40,000. This amount of data means we also have a great deal of qualitative observations of clinical disease, which also helped move us forward more quickly to emergency use.
Safety monitoring by the CDC and FDA will continue indefinitely, whether a vaccine has full licensure or emergency use authorization. We will be part of the ongoing CDC studies that follow use of the vaccine in emergency use and, later on, with full licensure through various observational studies.
With several different types of platforms for developing these vaccines, what does that mean for side effects?
Monto. There are mild acceptable side effects right after administration of these vaccines. Vaccines are sometimes reactogenetic, with your body letting you know with some fatigue, aching, fever, and soreness around the injection site—all typical adverse reactions. The dose finding part of vaccine development is to balance what is tolerable in terms of side effects and what gives you the best protection in terms of antibody development. As long as side effects are not severe, we are far less concerned, because we are dealing with risk-benefit between vaccine side effects and the well-known effects of COVID disease.
Martin. At this point, statistically, you certainly would want to consider getting the vaccine.
Monto. Right. We have not seen Guillain-Barre syndrome, which is sometimes reported with flu vaccines. We’ve seen very rare cases of Bell’s palsy, a facial paralysis. This also shows up with some vaccines, all at very low frequency. Bell’s palsy is also a side effect of COVID itself and probably occurs more frequently from getting COVID than from not getting COVID. And Bell’s palsy, like Guillain-Barre syndrome, occurs naturally in unvaccinated populations. So we might have a slight statistical excess in the vaccinated, but it is so rare that you have to vaccinate millions of people to demonstrate that slight excess. And thus far it really has not shown up as the vaccine is rolled out. Meanwhile, millions are getting protected against COVID, which affects far more people right now than Bell’s palsy. So the benefit far outweighs the risk, and people should get vaccinated without concern.
Every day that goes by, we know more about human immunity to this virus, whether from natural infection or from a vaccine.
—Emily Toth Martin
Again, as with any vaccine, in very rare cases anaphylaxis can occur just after receiving the vaccine. That’s why you need to stay at the vaccination site for 15-20 minutes after receiving any vaccine in case you have an allergic reaction.
How long will immunity last?
Martin. This is where observational studies come in, as we watch carefully how long protection continues for the millions of vaccines administered, mostly outside of clinical trials. Every day that goes by, we know more about human immunity to this virus, whether from natural infection or from a vaccine.
Monto. Warp Speed accelerated vaccine development. We have not put the same kind of resources into deployment and observation. We need a lot of attention given to the critical questions everybody wants to know about these vaccines. And you can’t get those answers from clinical trials, even if they involve fifty or sixty thousand participants. You won’t learn everything you can in that kind of population when you’re giving the vaccine to millions because not everyone will share their experience with you.
Should we vaccinate people who have had the disease to prevent reinfection?
Monto. My answer would be, yes but at a lower priority. Curiously, the antibodies produced by the vaccines are even higher than in people recovered from COVID, those with “natural immunity.” It has also been reported that asymptomatic and mild infection may produce less antibody than from severe infection. This is another important reason to vaccinate people with previous infections.
Martin. We’ve been saying that a coronavirus vaccine would have to beat nature and it seems to be doing that.

Monto. We’re not used to that, but it’s actually happening. Typically, natural immunity is better than that produced by vaccination. In our ongoing household study, we now have ten years of data on the seasonal coronaviruses—the four common coronaviruses that circulate seasonally and cause common colds in most people and more severe disease in some.
Martin. So we know there are reinfections. Human immunity to these seasonal coronaviruses wanes. The need for booster shots, like with flu, seems to be a real possibility going forward.
Monto. One individual in our study actually had three infections with a coronavirus, then became one of the first people in the group of households to become infected with SARS-CoV-2. This suggests that our antibodies have a limit. But we know from other viruses—flu in particular—that reinfection, once you have antibodies, is not as severe. Again, there is no downside to being vaccinated. A major upside is that, if there is waning of immunity, you’re likely to have a more mild disease if you do get infected.
How concerning are the variants?
Martin. Flu is a good segue to this question, because we hear each year with influenza how changes in the virus affect the efficacy of vaccines. All viruses shift and change. We pay close attention because those changes may make the virus interact differently with our immune system. With genetic changes in the COVID virus, how much will this impact the efficacy of vaccines?
Monto. As we continue to do sequencing of this virus worldwide, I am not overly worried. The virus is changing but not enough to fully escape the antibodies produced by the genetic messages in the vaccines. We have been living for years with four seasonal coronaviruses, the ones that cause common colds, and those viruses have been about the same for the fifty years I’ve been involved in studying them. That may mean that, when the virus isn’t spreading so much, variants won’t be as much of a problem.
Martin. We have a strong infrastructure in place to follow variants, because we watch the process unfold every year with flu. We monitor flu changes throughout the year—looking for mutations and variants, who gets infected, if they were vaccinated. This helps us understand not only how a vaccine is performing but all the minor adjustments we can make to optimize our response. The US does a remarkable job of monitoring all the vaccines we use in the population. We can use the same methods we use for the flu vaccines to figure out solid answers to these questions for COVID vaccines. Some of the variants do seem to be more transmissible.
Monto. Given how strong an immune response the vaccines are instigating, they should confer relatively strong protection against these new variants. As we see with flu, it is rare for a virus to completely evade vaccine protection this quickly. It could take years for a particular version of a vaccine to be entirely unhelpful against a particular strain of a virus. And we can always update the vaccine as necessary, as we do with flu.

Martin. The proteins of the virus don’t seem to be changing in a way that makes our body react differently to them. To our body, they look similar to the proteins that come out of the vaccine process. Each of the new variants has slightly different characteristics. Evidence is still emerging as to whether individual variants may cause disease that is more severe. Ultimately, we have to be even more effective with our public health mitigation efforts, from vaccine uptake to ongoing disease mitigation behaviors like wearing masks.
Monto. Right. By any standard for vaccines, the vaccines against COVID are a remarkable victory. We struggle to get people to understand that, during flu seasons, a 50% efficacy rate is still very good. The 94-100% efficacy for some COVID vaccines means only a few of those 100 individuals will get infected after receiving that particular vaccine. That means 98 or 99 individuals avoid having severe disease, hospitalization, death, and—with COVID—becoming long-haulers with loss of taste and smell, heart damage, neurological issues, and so on . . . we will have avoided those extremely negative outcomes entirely for 95% of the population that receives that vaccine.
Martin. And even with that 50/50 chance of getting flu, you can think of yourself not only as an individual but as someone who can spread flu to others. And if you think about how you and those others are at risk not only of a nasty bout with flu but potentially with hospitalization and death, then a 50% reduction of that is certainly worth every injection, especially given how easy it is for most of us to receive a flu shot.
Monto. Many of us live with young children, older adults, or people with immune conditions in our homes or interact with people in those populations at work or in other social settings. If we get flu or COVID, we put at risk those people and others we might not know.
Martin. We are always asking people to take a community view of disease transmission, in addition to the precise numbers we can offer about their own individual chance of contracting a disease if vaccinated. Vaccines are very important, as are the other safety measures for preventing the spread of disease. By using all of the public health tools available to us as individuals and as communities, we can move more quickly toward an end to this pandemic.
Ask the Experts
What if I’m pregnant?Monto. We’ve not done clinical safety studies in pregnant people because of concerns around liability issues. So for many years, we did not specifically recommend influenza vaccines for pregnant people when influenza vaccine was recommended based on risk categories. With the 2009 swine flu pandemic, we saw that pregnant people contracting H1N1 were at higher risk of early labor and severe pneumonia. We now recommend vaccinating pregnant people and know from years of observational studies that it is safe for them.
Martin. And with the COVID-19 vaccines, it looks like pregnant people react similarly to the rest of the population. So we expect them to work just like other approved vaccines.
Monto. We do many observational studies at HIVE. Given how few people will want to be in placebo groups with COVID, we will have to rely on observational studies to give us the additional information we need going forward.
What about kids?
Martin. We had an early, incomplete takeaway that children weren’t getting infected, and
that looks more like an epidemiological rather than an immunological phenomenon. But
I think that set the stage for moving slower with vaccine trials for children. The
16 and 17 year olds as a population are important in terms of transmission—mobile,
interact often with others, tend to have jobs where they interact with the general
public.
With influenza, school-aged children are the spreaders in the population. Prioritizing them can really bring an epidemic under control more rapidly. We aren’t
having this discussion with COVID yet because we don’t see that much symptomatic infection in young individuals. But asymptomatic infection is playing a much bigger role than we thought with this virus. This is
an argument for quickly vaccinating younger people. You can vaccinate the people spreading
the disease, even though they may not themselves be impacted as severely by the disease.
You can vaccinate first the people most likely to become severely ill. Or you can
focus on your critical infrastructure, vaccinating the people you need to keep your
hospitals moving. We started there with this pandemic, because hospitals were so overwhelmed.
What do you make of the pause on the Johnson & Johnson vaccine?
Monto. First of all, the pause shows how carefully safety is being considered. If there
is any indication of a potential—not even a proven—side effect, the program is paused.
The program was paused following reports of six cases of cerebral venous sinus thrombosis
(CVST) after about 7 million doses of the vaccine had been administered. Once the
situation was fully examined, 15 cases were found—a rate of 2-3 cases per million
vaccinations received. It occurred mainly in women under age 59. Because nearly all
cases occurred 7-13 days after vaccination and only in the US, it was thought that
it could be vaccine related. Because the benefits of vaccination clearly outweighed
the very low risk, it was decided to continue the use of this vaccine but also inform
the public of the very low risk. And physicians were made aware of ways to treat the
syndrome, if seen, different from standard ways of handling ordinary thrombotic episodes.
Martin. This is an important vaccine. It is safe and effective and has several logistical
advantages over the Pfizer and Moderna vaccines—including its single-dose administration
and the fact that it does not rely on cold storage. When you think about the need
for COVID vaccines around the world, in many places where transportation and cold-storage
access are a challenge, the Johnson & Johnson vaccine’s advantages make it very important.
If I’m vaccinated, should I still get tested if I have symptoms or think I was exposed to someone with COVID-19?
Martin. Yes. We have a lot to learn yet about how these vaccines prevent transmission, especially asymptomatic transmission. The data we have now is based on studies in millions of individuals. We’re now administering vaccines to hundreds of millions. We have to continue tracking cases, general disease outcomes, and the transmission of particular variants in order to understand the vaccines’ effectiveness and as well as asymptomatic transmission. Tracking and understanding asymptomatic transmission is especially important with COVID because of the danger of ongoing transmission in this pandemic. The reality is that vaccines almost certainly reduce asymptomatic transmission significantly, but we really can’t tell by how much without good testing.
The insights expressed in this article are current as of April 2021. Learn more about the School of Public Health’s most recent findings on COVID-19 and related studies on the Coronavirus News Center.
- Interested in public health? Learn more today.
- Read Good Science Changes: That’s a Good Thing in this issue of Findings.
- Support research and engaged learning at Michigan Public Health.
