Sleep Awareness Week: A Chance to Adjust and Prioritize Sleep

Astrid Zamora and Erica Jansen
Are you still feeling the effects of the Daylight Saving Time (DST) shift? If so, you are not alone. Experts say it can take the body about one week to readjust to this one-hour change in schedule (read more here about why sleep experts recommend abandoning this time shift).1 While you are readjusting might be a good time to assess your sleep health and prioritize good sleep habits.
What is “sleep health”?
Adequate sleep duration is only one aspect of restorative and health-promoting sleep. A more holistic concept, sleep health encompasses a “multidimensional pattern of sleep-wakefulness, adapted to individual, social, and environmental demands, that promotes physical and mental well-being.”2 Good sleep health includes:
- being personally satisfied with sleep
- appropriate timing (consistent and aiming for bedtime before midnight)
- adequate duration (7-9 hours for adults)
- high efficiency (asleep for at least 85% of total time in bed)
- sustained alertness during waking hours
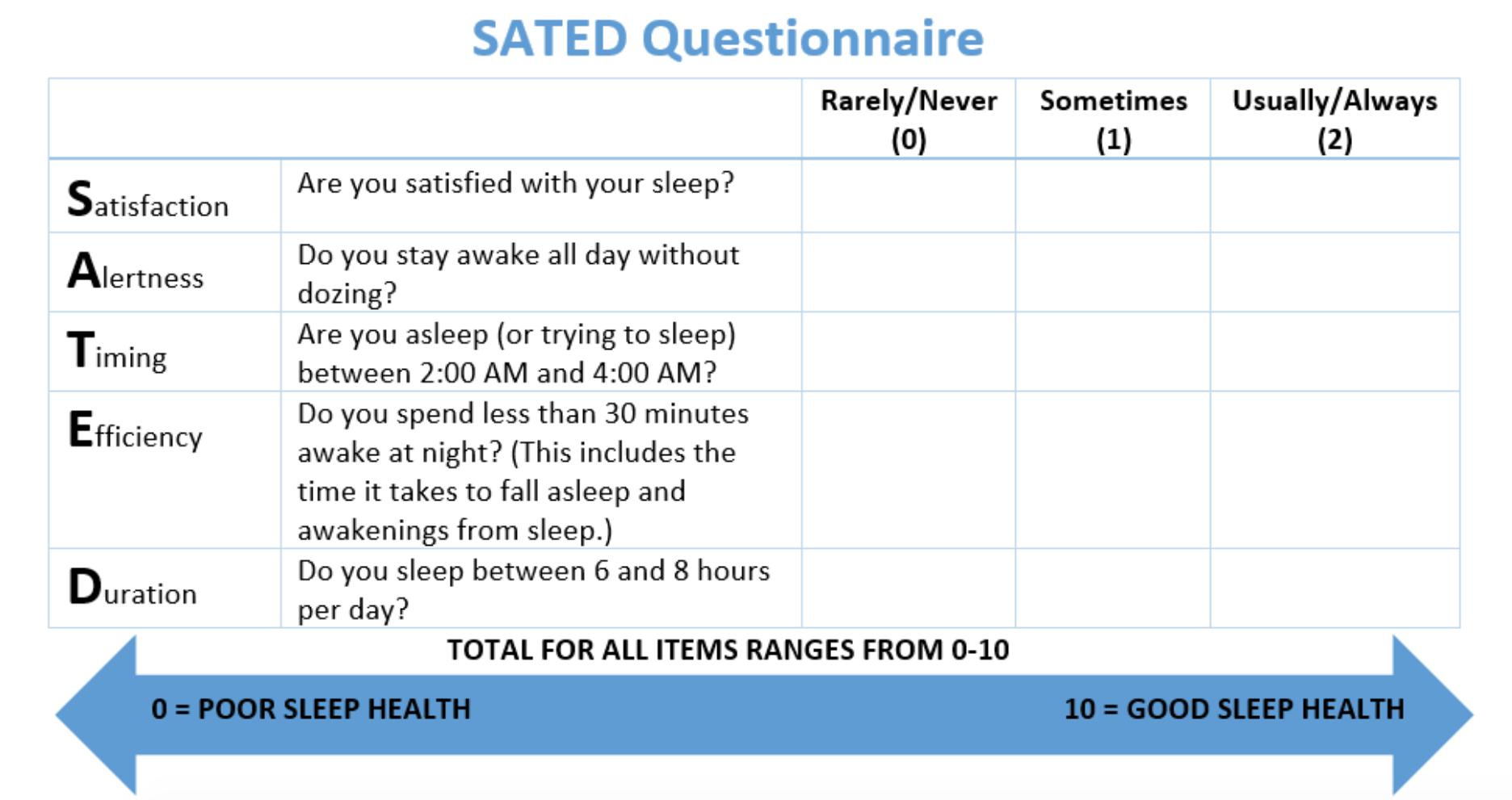
Fill out the SATED questionnaire2 below to determine your sleep health score.
How healthy is our sleep at a population level?
A recent study found that the prevalence of short sleep duration among US adults was 36%3 while an estimated one-third experienced chronic insomnia—difficulty falling asleep or staying asleep.4 CDC data show that the prevalence of short sleep duration among college students is much higher, with about two-thirds of 18–24 year-olds not meeting recommended guidelines for sleep duration.5 Other studies point to a higher prevalence of insomnia in young adult populations as well.6
What about graduate students, and what about during the pandemic?
Interestingly, recent evidence shows that COVID-19 stay-at-home restrictions have resulted in longer sleep duration among college students.7 Pandemic restrictions have reduced the mismatch between external (social) and internal (biological) sleep-wake timing as people have more flexibility to choose their sleep schedules.8,9 Importantly, this reduction in mismatch has led to less “social jetlag”—a large difference in sleep timing between weekends and weekdays associated with poor cardiometabolic effects. On the flip side, terms such as coronasomnia or covidsomnia have been coined to illustrate the negative impact COVID-19 has had on sleep quality and insomnia symptoms experienced by many10–12 due to increased stress, uncertainty, and illness.
How can we improve our sleep health?
- MHealthy has put together a list of tips for restful sleep that not only promote healthier sleep overall but can be applied to help cope with
DST changes and the ongoing pandemic.
- In addition to these tips, our recent research shows that higher dietary quality throughout the day, notably higher fruit and vegetable intake, may be beneficial for improving sleep quality and insomnia symptoms.6,13–15
- Join the MHealthy Sleep Challenge
- For more information on improving overall sleep health, we encourage University of Michigan School of Public Health benefits-eligible faculty and staff to sign up for the MHealthy Sleep Challenge.
References
- Roenneberg T, Wirz-Justice A, Skene DJ, et al. Why Should We Abolish Daylight Saving Time? J Biol Rhythms. 2019;34(3):227-230. doi:10.1177/0748730419854197
- Buysse DJ. Sleep health: can we define it? Does it matter? Sleep. 2014;37(1):9-17. doi:10.5665/sleep.3298
- Khubchandani J, Price JH. Short Sleep Duration in Working American Adults, 2010–2018. J Community Health. 2020;45(2):219-227. doi:10.1007/s10900-019-00731-9
- Morin CM, LeBlanc M, Daley M, Gregoire JP, Mérette C. Epidemiology of insomnia: Prevalence, self-help treatments, consultations, and determinants of help-seeking behaviors. Sleep Med. 2006;7(2):123-130. doi:10.1016/j.sleep.2005.08.008
- CDC - Data and Statistics - Sleep and Sleep Disorders. Published March 5, 2019. Accessed March 8, 2021. https://www.cdc.gov/sleep/data_statistics.html
- Jansen EC, She R, Rukstalis MM, Alexander GL. Sleep Duration and Quality in Relation to Fruit and Vegetable Intake of US Young Adults: a Secondary Analysis. Int J Behav Med. Published online February 3, 2020. doi:10.1007/s12529-020-09853-0
- Benham G. Stress and sleep in college students prior to and during the COVID-19 pandemic. Stress Health. n/a(n/a). doi:https://doi.org/10.1002/smi.3016
- Gruber R, Saha S, Somerville G, Boursier J, Wise MS. The impact of COVID-19 related school shutdown on sleep in adolescents: a natural experiment. Sleep Med. 2020;76:33-35. doi:10.1016/j.sleep.2020.09.015
- Blume C, Schmidt MH, Cajochen C. Effects of the COVID-19 lockdown on human sleep and rest-activity rhythms. Curr Biol. 2020;30(14):R795-R797. doi:10.1016/j.cub.2020.06.021
- Huang Y, Zhao N. Generalized anxiety disorder, depressive symptoms and sleep quality during COVID-19 outbreak in China: a web-based cross-sectional survey. Psychiatry Res. 2020;288:112954. doi:10.1016/j.psychres.2020.112954
- Li Yun, Qin Qingsong, Sun Qimeng, Sanford Larry D., Vgontzas Alexandros N., Tang Xiangdong. Insomnia and psychological reactions during the COVID-19 outbreak in China. J Clin Sleep Med. 16(8):1417-1418. doi:10.5664/jcsm.8524
- Wright KP, Linton SK, Withrow D, et al. Sleep in university students prior to and during COVID-19 Stay-at-Home orders. Curr Biol. 2020;30(14):R797-R798. doi:10.1016/j.cub.2020.06.022
- Jansen EC, Baylin A, Cantoral A, et al. Dietary Patterns in Relation to Prospective Sleep Duration and Timing among Mexico City Adolescents. Nutrients. 2020;12(8):2305. doi:10.3390/nu12082305
- Jansen EC, Stern D, Monge A, et al. Healthier dietary patterns are associated with better sleep quality among midlife Mexican women. J Clin Sleep Med. Published online August 15, 2020. doi:10.5664/jcsm.8506
- Jansen EC, She R, Rukstalis M, Alexander G. Changes in fruit and vegetable consumption in relation to changes in sleep characteristics over a 3-month period among young adults. Sleep Health. In press. Sleep Health. In Press. 2021.
About the Authors
 Astrid Zamora is a PhD candidate in Nutritional Sciences at the University of Michigan
School of Public Health. Her research seeks to understand how environmental exposures,
such as endocrine-disrupting chemicals (EDCs), pesticides, and diet influence adolescents
and women’s sleep and metabolic health. She earned an MPH from the University of California,
Berkeley and a BS from the University of California, Davis.
Astrid Zamora is a PhD candidate in Nutritional Sciences at the University of Michigan
School of Public Health. Her research seeks to understand how environmental exposures,
such as endocrine-disrupting chemicals (EDCs), pesticides, and diet influence adolescents
and women’s sleep and metabolic health. She earned an MPH from the University of California,
Berkeley and a BS from the University of California, Davis.

