Balancing heritage and health: Significance of culturally tailored dietary recommendations for immigrant communities

Shichi Dhar
BS ‘24, Public Health Sciences
Food carries a significance that extends beyond sustenance; it represents culture, identity, and the legacy of generations. For immigrants, culinary traditions provide a connection to their roots and comfort in a new place. But when faced with the need to manage chronic conditions like type 2 diabetes, striking a balance between health and heritage becomes a challenge. Recognizing this, there's a growing acknowledgment of the importance of culturally tailored dietary guidance that resonates with individual lifestyles.
The Cultural Importance of Food
For many people who have immigrated to a new country, a meal is more than just the food on a plate—it's a little piece of home. When provided with alternative diets that do not align with cultural norms to manage type 2 diabetes or other conditions, many immigrants are forced to choose between their culture and their health—minimizing the effectiveness of dietary counseling and adherence. The one-size-fits-all approach to nutrition often fails because it doesn't consider the cultural and traditional importance of food.
The Evidence for Customization
Research shows that immigrant populations, specifically South Asian Americans, demonstrate a high prevalence of type 2 diabetes, a leading cause of illness and death. This population also tends to demonstrate earlier onset of type 2 diabetes and health complications attributed to the condition. With an estimated 70 million South Asians affected by diabetes—a number projected to escalate to 121 million by 2030—understanding the intricate interplay between culture and health becomes critically important. Studies reveal that lifestyle changes, including dietary optimization, significantly impact diabetes management, stressing the need for both sustainable and successful dietary interventions.
Adapting Diets, Not Erasing Them
Instead of eliminating familiar foods or suggesting radical dietary overhauls, health strategies should aim to modify existing meals to create holistically healthier food that aligns with dietary recommendations. For example, modifications of traditional South Asian dishes involving the use of whole grains, lentils, and nutrient-rich vegetables have been shown to provide a more diabetes-friendly meal without losing its cultural significance.
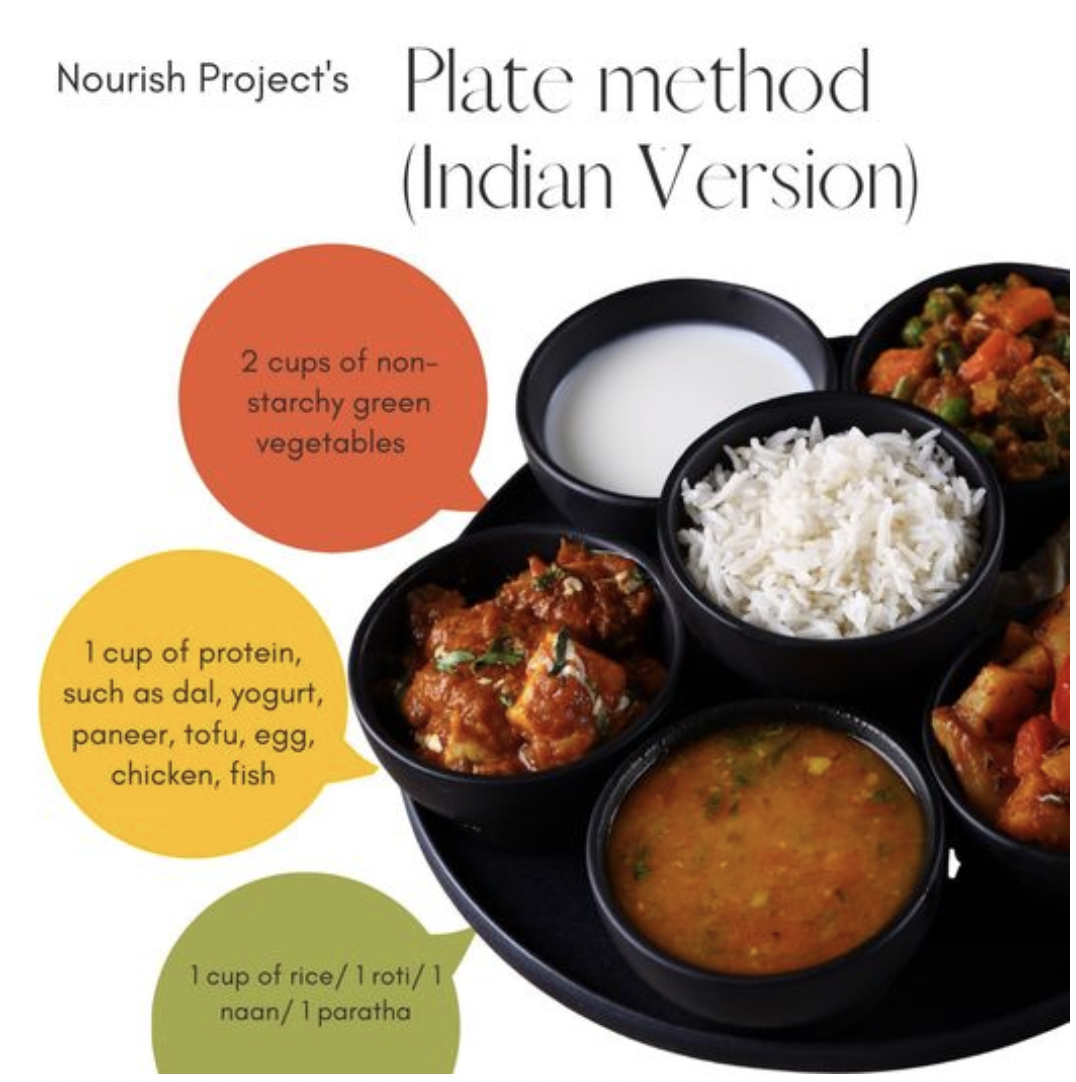
Consider the ubiquitous Indian dish of dal, a staple in many South Asian homes. A simple modification such as using a mix of whole pulses (lentils, beans, or peas) rather than split ones can improve the fiber content, leading to slower digestion and better blood sugar control. In addition, adding a variety of non-starchy vegetables to the dish not only enhances its nutritional profile but also retains its traditional essence.
The Human Element in Health
It is not about prescribing a diet; it is about personalizing the dietary experience for better health benefits. Culturally sensitive nutrition education has led to improved adherence to modified diets, demonstrating that people are more inclined to make changes that respect their traditions and preferences.
When addressing dietary management of type 2 diabetes, people-first recommendations are crucial. Alterations in diet for the management of diabetes need not negate one’s cultural and culinary identity. These modifications should act as enablers, encouraging individuals to make health-conscious choices without forfeiting traditional foods.
Overall, personalized dietary advice is more effective than generic advice in chronic disease self-management. The intersection of culture and health is profound, and particularly evident in immigrant populations. For healthcare providers and educators, recognizing the indivisible nature of cultural identity and food when creating dietary recommendations can lead to better adherence and a healthier, happier life for those managing type 2 diabetes. By understanding and integrating culturally relevant food, we pave the way for a care model that embraces both heritage and health to be both successful and sustainable.
ABOUT THE AUTHOR
 Shichi Dhar, BS ‘24, is a graduate of the Public Health Sciences program at the University
of Michigan School of Public Health. She is interested in preventative medicine and
learning how to make health-improvement interventions sustainable for communities
of color. A fun fact about Shichi is that she loves to travel and try foods from all
over the world.
Shichi Dhar, BS ‘24, is a graduate of the Public Health Sciences program at the University
of Michigan School of Public Health. She is interested in preventative medicine and
learning how to make health-improvement interventions sustainable for communities
of color. A fun fact about Shichi is that she loves to travel and try foods from all
over the world.
- Resources on South Asian cuisine and culturally sensitive dietary modifications
- Learn more about Nutritional Sciences at Michigan Public Health.
- Learn more about the Undergraduate Program at Michigan Public Health.
