What the Polio Epidemic Can Teach Us about Vaccine Hesitancy
Samantha Kasselman, Ryan Olivier, Hadley Wallace, Claire Gleason, and Kerry Lindquist
Bachelor’s Students in Public Health
The Story of Jackie Wallace
"They told me I was going to die. I was given last rites three times.”
–Jackie Wallace
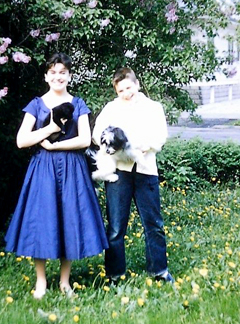
While researching the poliovirus over the past semester, we had the unique opportunity to interview Jackie Wallace on her experience contracting the virus just before the polio vaccine was released. Jackie Wallace is the grandmother of Hadley Wallace, a bachelor’s degree student and one of the authors of this article. This interview shed light on the individual experience of having a crippling disease and the extraordinary role vaccines play in public health.
 It was the summer of 1951. Jackie Wallace was two months shy of 15. She had just returned
home from a camping trip when she began to have a mild fever and dull headache. We
were in awe to hear that a mere week later, she lay paralyzed and unconscious in an
overflowing Chicago hospital ward. Jackie had been diagnosed with polio and was fighting
for her life.
It was the summer of 1951. Jackie Wallace was two months shy of 15. She had just returned
home from a camping trip when she began to have a mild fever and dull headache. We
were in awe to hear that a mere week later, she lay paralyzed and unconscious in an
overflowing Chicago hospital ward. Jackie had been diagnosed with polio and was fighting
for her life.
The virus engulfed Jackie’s body from head to toe, causing her to remain encased in an iron lung for the next six months. She was caught in a vicious cycle of befriending new patients in her hospital room only to watch them die weeks later. Against all odds, Jackie overcame polio. Today, she says her wheelchair serves as an unwelcome reminder of the crippling illness that struck her almost 70 years ago. With the COVID-19 vaccine being the center of today’s news cycle, she wanted to emphasize the importance of immunizations: “I know the value of vaccines,” Jackie quietly stated. "I got my children vaccinated as soon as possible. No question."
What Does It Mean to Be Vaccine Hesitant?
Vaccines are an undeniably effective method of protecting both individuals and entire populations from infectious diseases. Though they were once viewed as proof of medical innovation and advancement, in recent years, individual attitudes toward vaccines have shifted in a negative direction. The term vaccine hesitancy describes those who harbor varying degrees of skepticism or fear toward the efficacy and safety of vaccines.
The development and severity of vaccine hesitancy is individualized and depends on one’s exposure to various social, political, and environmental influences.1 For this reason, it is difficult to predict patterns of vaccine hesitancy and effectively inform vaccine-hesitant individuals of the dangers associated with avoiding vaccination.
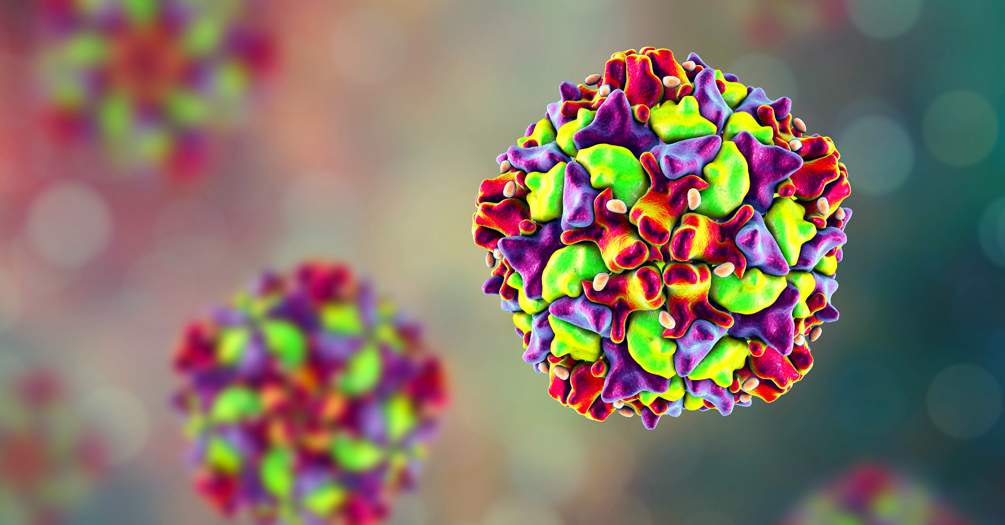
The polio vaccine is just as essential to protecting public health today as it was during the 1950s.
Jackie Wallace’s story reminds us that technological advances in medicine—especially vaccines—are not to be taken for granted. The polio vaccine is just as essential to protecting public health today as it was during the 1950s.
What Risks Are Associated with Vaccine Hesitancy?
Even before the COVID-19 pandemic ravaged the globe, rising vaccine hesitancy had resulted in decreased immunization coverage in the US across multiple vaccine-preventable diseases, including measles, polio, and diphtheria. Vaccine-hesitant individuals threaten to reverse the progress that has been made in tackling vaccine-preventable diseases.2
A parent who is vaccine-hesitant and ultimately decides not to vaccinate their new baby against polio increases their child’s risk of contracting the disease
Rabindra Abeyasinghe, a World Health Organization representative in the Philippines, has noted how coverage for three doses of the oral polio vaccine administered to children younger than one year of age dropped from 71% in 2017 to 68% in 2018, the lowest in the past five years.3 Many countries that had achieved polio eradication or were very close to eradication have seen a resurgence in cases, attributable largely to vaccine-hesitancy.3 Research shows that vaccine-hesitant parents far outnumber vaccine refusers4 but that the proportion of parents categorized as vaccine-hesitant may be increasing.5
 Polio was eliminated in the US over 30 years ago—meaning there is no ongoing transmission
of the virus.6 But a parent who is vaccine-hesitant and ultimately decides not to vaccinate their
new baby against polio increases their child’s risk of contracting the disease.7
Polio was eliminated in the US over 30 years ago—meaning there is no ongoing transmission
of the virus.6 But a parent who is vaccine-hesitant and ultimately decides not to vaccinate their
new baby against polio increases their child’s risk of contracting the disease.7
And the risks of vaccine hesitancy extend far beyond the direct consequences of developing a vaccine-preventable illness. Because no cure for paralytic polio exists, the main focus is on increasing the patient’s comfort levels and preventing further complications.8 Treatment options such as pain relievers or portable ventilators to assist breathing are very costly, especially if the patient is reliant on them for a long period of time.7 However, the cost of receiving the polio vaccine is far less economically burdensome, as most health insurance plans cover the cost of vaccines.9
Vaccinations Are More Important Today than Ever Before
The sheer urgency of the COVID-19 pandemic, combined with advances in vaccine technology and clinical trial design, has resulted in the development of multiple COVID-19 vaccines at an unprecedented speed. Pharmaceutical companies—including Pfizer, Moderna, and AstraZeneca—claim to have developed vaccines with 90-95% effectiveness in creating an immune response to the SARS-CoV-2 virus. This level of efficacy is on par with that of polio vaccines, which are upward of 90% effective at preventing infection with the poliovirus, depending on dosage.10
Vaccine hesitancy plays a major role in the effort to end the COVID-19 pandemic. A recent survey suggests only 51% of Americans would be willing to receive the COVID-19 vaccine.11 Now that the Pfizer and Moderna vaccines have been approved by the Food and Drug Administration (FDA), it is imperative that individuals get vaccinated in order to reduce the number of cases and deaths caused by COVID-19.
We recommend that individuals who are hesitant to receive the COVID-19 vaccine begin by researching the efficacy of these vaccines using credible sources. We encourage individuals to read about available clinical trial research to understand what public health officials say about the COVID-19 vaccines. It also may be helpful for individuals to familiarize themselves with the Center for Disease Control and Prevention’s recommendations regarding vaccination.
We all should make a conscious effort to avoid misinformation spread by social media and less reputable websites. You have the ability to protect yourself and your community by getting vaccinated in a timely manner.
A Life That Could Have Been
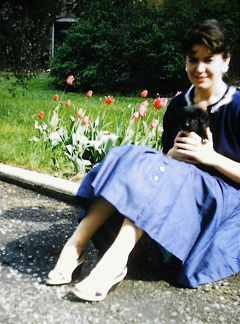 “I would have been a runner. I would have finished high school and gone to college
in California. My life would have been very different,” Jackie told us while reflecting
on how her life would have dramatically changed if she had been able to receive the
polio vaccine as a child. Today, Jackie wants everyone to know that “getting vaccinated
is a blessing.”
“I would have been a runner. I would have finished high school and gone to college
in California. My life would have been very different,” Jackie told us while reflecting
on how her life would have dramatically changed if she had been able to receive the
polio vaccine as a child. Today, Jackie wants everyone to know that “getting vaccinated
is a blessing.”
There is an immense burden associated with contracting a preventable disease. Jackie Wallace dealt with physical, emotional, social, and financial hardship as a result of her polio diagnosis. The obstacles she was forced to overcome could have been alleviated through the availability of a polio vaccine. We highly encourage readers to consider the health and well-being of themselves and those closest to them when choosing whether to receive future vaccines.
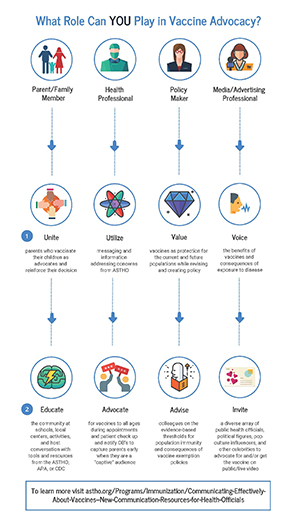
What Can You Do?
Notes
- Larson, Jarrett, Eckersberger, Smith, and Paterson. "Understanding Vaccine Hesitancy around Vaccines and Vaccination from a Global Perspective: A Systematic Review of Published Literature, 2007-2012." Vaccine 32/19 (17 April 2014):2150–2159.
- Bliss and Morrison. "The Risks of Misinformation and Vaccine Hesitancy within the Covid-19 Crisis." Center for Strategic and International Studies, September 4, 2020.
- Ravelo, Jenny Lei. "Another Casualty of Vaccine Hesitancy: Philippines Declares Polio Outbreak." Devex September 19, 2019.
- Shen and Dubey. "Addressing Vaccine Hesitancy: Clinical Guidance for Primary Care Physicians Working with Parents." Canadian Family Physician 65/3 (March 2019):175-181.
- Dubé, Vivion, and Macdonald. "Vaccine Hesitancy, Vaccine Refusal, and the Anti-Vaccine Movement: Influence, Impact, and Implications." Expert Review of Vaccines 14/1 (January 2015):99-117.
- Polio Elimination in the United States. Centers for Disease Control and Prevention, October 25, 2019
- Making the Vaccine Decision: Addressing Common Concerns. Centers for Disease Control and Prevention, August 5, 2019.
- Polio: Diagnosis and Treatment. Mayo Clinic, December 1, 2020.
- Polio Vaccination: What Everyone Should Know. Centers for Disease Control and Prevention, May 4, 2018.
- Polio Vaccine Effectiveness and Duration of Protection. Centers for Disease Control and Prevention, May 4, 2018.
- Jackson, Newall, and Yi. "Most Americans Not Expecting to Be Back to Bormal until Summer at the Earliest." Ipsos, February 2, 2021.
About the Authors
 Samantha Kasselman is a senior in the Bachelor of Science program at the University
of Michigan School of Public Health. Previously, she collaborated with PhD fellows
and MDs at Michigan Medicine on a research project providing a potential pathway to
intervention among patients at risk for pancreatic cancer development. She is currently
a research assistant with Dr. Minal Patel at the Collaborative for Behavioral Solutions
to HealthCare Engagement and Access (CBSHC). Her areas of interest include disease
prevention, medical innovation, and health education.
Samantha Kasselman is a senior in the Bachelor of Science program at the University
of Michigan School of Public Health. Previously, she collaborated with PhD fellows
and MDs at Michigan Medicine on a research project providing a potential pathway to
intervention among patients at risk for pancreatic cancer development. She is currently
a research assistant with Dr. Minal Patel at the Collaborative for Behavioral Solutions
to HealthCare Engagement and Access (CBSHC). Her areas of interest include disease
prevention, medical innovation, and health education.
 Kerry Lindquist is a senior at the University of Michigan School of Public Health
pursuing a Bachelor of Arts in Community and Global Public Health. She is particularly
interested in learning how to improve our health delivery system through advocacy,
education, and research. Lindquist is passionate about the research she does for the
Center for Healthcare Outcomes and Policy (CHOP), where she works under the direction
of Dr. Dana A. Telem, assisting with interviews on topics including bariatric surgery
attrition rate and workplace conflict among surgical teams.
Kerry Lindquist is a senior at the University of Michigan School of Public Health
pursuing a Bachelor of Arts in Community and Global Public Health. She is particularly
interested in learning how to improve our health delivery system through advocacy,
education, and research. Lindquist is passionate about the research she does for the
Center for Healthcare Outcomes and Policy (CHOP), where she works under the direction
of Dr. Dana A. Telem, assisting with interviews on topics including bariatric surgery
attrition rate and workplace conflict among surgical teams.
 Hadley Wallace is a senior studying Public Health and Linguistics at the University
of Michigan. During her time at the university, Hadley has developed a passion for
research and development of preventative solutions in healthcare. Upon graduation
she plans on pursuing a master’s degree in Speech-Language Pathology and will work
toward incorporating an instream public health approach into her clinical care.
Hadley Wallace is a senior studying Public Health and Linguistics at the University
of Michigan. During her time at the university, Hadley has developed a passion for
research and development of preventative solutions in healthcare. Upon graduation
she plans on pursuing a master’s degree in Speech-Language Pathology and will work
toward incorporating an instream public health approach into her clinical care.
 Claire Gleason is a junior in the Bachelor of Science program at the University of
Michigan School of Public Health. She is involved in research looking into the relationships
between ketogenic diets and metabolic health in Dr. Dave Bridges’ nutritional sciences
lab and is a Peer Facilitator for the Undergraduate Research Opportunity Program,
supporting prospective student researchers with academic and professional guidance.
Claire Gleason is a junior in the Bachelor of Science program at the University of
Michigan School of Public Health. She is involved in research looking into the relationships
between ketogenic diets and metabolic health in Dr. Dave Bridges’ nutritional sciences
lab and is a Peer Facilitator for the Undergraduate Research Opportunity Program,
supporting prospective student researchers with academic and professional guidance.
 Ryan Olivier is a junior studying Public Health Sciences at the University of Michigan
School of Public Health. He works as a research assistant to Professor Pierre F. Apostolides
at the Kresge Hearing Research Institute and, after graduation, plans to pursue a career in medicine with a public health
focus, using his understanding of the social determinants of health and health care
inequalities to improve patient care.
Ryan Olivier is a junior studying Public Health Sciences at the University of Michigan
School of Public Health. He works as a research assistant to Professor Pierre F. Apostolides
at the Kresge Hearing Research Institute and, after graduation, plans to pursue a career in medicine with a public health
focus, using his understanding of the social determinants of health and health care
inequalities to improve patient care.
- Interested in public health? Learn more here.
- Read more articles about infectious disease.
- Support research and engaged learning at the School of Public Health.