Meet Alice: Precision Health at Michigan Public Health

Sharon Kardia
Millicent W. Higgins Collegiate Professor of Epidemiology
 You've actually met Alice already. She's on the cover of this issue with her mother
and grandmother. They're also on the facing page, where you can read a bit about them
and some of the basic information that could be entered into a precision health database.
You've actually met Alice already. She's on the cover of this issue with her mother
and grandmother. They're also on the facing page, where you can read a bit about them
and some of the basic information that could be entered into a precision health database.
How do we take trillions of data points from hundreds of millions of people and use that to inform a treatment plan for an individual patient? And how do we get all that data from those hundreds of millions of people in the first place?
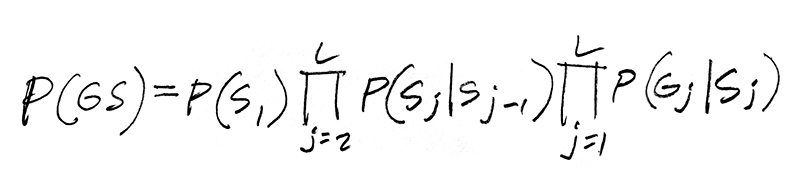
Public health is centered around the flow of information from individuals to communities and back to individuals. Practitioners and researchers look for health trends—large and small—and use various methods to identify disease and improve outcomes, building bridges between population-wide data and the treatment of individual patients. Whenever possible, public health practitioners collect data from entire populations to get the most complete pictures possible of population health. Most researchers do not have access to government data sources and have to recruit people into studies one participant at a time—and this is especially true of genetic research.
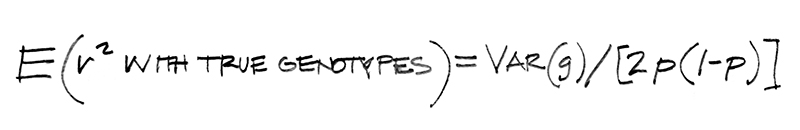
Some of the most important data we have for Alice and her family is genetic data. The most helpful genetic information we have about Alice's grandmother's diabetes diagnosis will come from subpopulations in England, in the Chippewa community, and in any subpopulations related to these groups regardless of geographic location. Alice's mother also has diabetes, and her vital genetic information will come from subpopulations in Germany, in England and the Chippewa community, and in any subpopulations related to these groups regardless of geographic location. If Alice is diagnosed with diabetes, her physicians will hope to access data from all of these sources as well as from subpopulations in the Netherlands and from those with Dutch heritage.
Genomes and Epigenomes
Reimagining definitions of place and time is a big part of advancing the power of precision health, especially when it comes to genomics. We can think of a population as a group of people living in a particular geographic location, and this will tell us a lot about their environmental, behavioral, and social health profiles. But their genetic profile is not geographically constrained in the same way. Each of our genomes stretches back through time and across continents to our various ancestors, with all the migrations and mutations that have occurred along the way.
Some of the data here indicate potential health risks for Alice and her family. Alice's grandmother is genetically predisposed to heart disease, which means Alice and her mother are too. Alice's mom had a recurrence of foot pain while pregnant with Alice and took aspirin for several weeks. And Alice's grandmother experienced a silica exposure while pregnant with Alice's mom, which would affect not only her grandmother's and her mother's health but also Alice's—because the egg that would become Alice spent time in Alice's grandmother's body as it was forming within Alice's mother's body.
Chronology matters beyond the broad sweep of time when we and our genes were evolving into the complex beings we are today. Environmental and social factors have impacts on our genes and therefore on our health, down to the minutes and seconds it might take us to consume food, run a mile, receive and process a bad piece of news, or experience a brief but severe toxicant exposure.
The epigenome—the chemical signals on our chromosomes and DNA—is sensitive to our internal and external physical realities. What we eat, how stressed we get, where we live and what we breathe, whether we exercise, and exactly when all of this happens can have tremendous effects on our genes by way of epigenetic factors.
Outcomes for the Sick
One of public health's major contributions is that it always wants to know why someone got sick. Was it the air, water, workplace, genes, lifestyle choices, a combination of these things? We have to document all of this vigilantly before we can aggregate information from individuals into enough data that lets us begin to understand the full health profile of an individual patient, their family, and the larger subpopulations in which they live.
Alice's arrhythmia flares up more often now that she has joined a soccer league. She loves spending time with her friends but is frustrated with the heart stuff, which makes her a little stressed out at school on days when she has practice or a game. The exercise, the arrhythmia, and the stress are all factors in Alice's ongoing health, including the state of her epigenome.
In clinical settings, precision health is already helping physicians by providing clinical decision supports (CDS), data-driven suggestions about treatments for individual patients. A CDS might be a genetic indication that one particular treatment will be more successful than another. Or it might be an alert that a particular drug is less likely to succeed with a patient or, alternatively, is likely to create a side effect or a substance addiction problem for them.
Imagine how much more accurate Alice's treatment could be if her physicians had access to genomic data from a much larger population than the community in which Alice currently lives, a population that would include people more closely related to Alice genetically than those living in her town. What treatments are most likely to alleviate Alice's arrhythmia? What drugs might work best for her? What do we know about Alice's family's lifestyle that could be contributing to or mitigating the problem?
Preventing Disease
By combining information about a family's history, lifestyles, environments, and social realities, researchers and practitioners can also assess and even predict disease with a great deal of accuracy.
The public health community is hoping precision health tools can help Alice, her family, and her physicians keep Alice healthy and minimize the effects of her heart condition.
We have many ways to know precise things about patients. Public health researchers in environmental health sciences, nutritional sciences, health behavior and health education, and health management and policy all are doing major projects in precision health. At the moment, genomics and epigenomics—the purview of statistical genetics and genetic epidemiology—remain the primary thing Michigan Public Health is doing to advance precision health. But other fields are rapidly getting involved.
Gonçalo Abecasis, Michael Boehnke, Bhramar Mukherjee, and other biostatisticians at Michigan Public Health are leading the world in genomic research and the construction of enormous population-wide databases of biomedical information. A helpful analogy is to think of their work as developing those bright yellow Dewalt tools we see at nearly every construction site. Nearly everyone in the world is using the precision health tools Abecasis, Boehnke, Mukherjee, and others are creating here at Michigan Public Health.
How can Alice's information help doctors treat people Alice will never meet? Should her family participate in a program like Genes for Good—one of the genomic databases Abecasis and his team are building?
As these top researchers work to create biomedical data archives for larger and larger populations, not only will we see improvements in clinical treatments, but we will actually begin to know who might get sick. And when we know that, we can create precise, localized preventive interventions that will keep some from getting sick in the first place and reduce the severity of illness for others. In addition to keeping more people healthy and reducing human suffering in many ways, these interventions create cost savings for all.
Overcoming Challenges
The physiological, logistical, and legal processes involved in collecting biomedical and other personal medical information at this level are complicated.
Alice's mother remembers the cell-phone smoking-cessation program that helped her mother recover from a relapse into smoking when Alice was born. It was this positive experience with technology that convinced her to consider getting her genome information through the Michigan Genomic Initiative. Still, Alice's grandmother is suspicious of big databases.
As precision health informs clinical and preventive outcomes, we will need more public communication and education about how big data impacts public health. Maintaining confidentiality and respecting privacy are legally mandated—we will still need data-collecting organizations to be transparent beyond what is legally required.
Alice recently took out school library books about how genes work and how they can help us learn about ourselves and our families. Alice and her mom started talking about Alice signing up with Genes for Good when Alice is a little older.
Sequencing the genome and collecting genetic data from thousands of people are vital to advancing precision health. So are the thousands of environmental and policy studies that public health researchers contribute every year. Working together across departments, schools, universities, public and private sectors, and even across borders, we can begin to discern much more accurate measures for keeping entire populations healthier as well as discerning much more accurate therapies for particular patients with a particular disease profile.
So what is precision health? In many ways it is nearly synonymous with public health and has been around since physicians centuries ago began looking beyond individual patients to see the path of an infectious disease through a local population. Precision health can improve much older and simpler problems, like bridging public health and other medical research with clinical practice. For good reasons—most obviously time and energy—physicians are limited in their ability to study and absorb the vast amounts of scientific research produced by health researchers around the world. Population-wide, patient-oriented precision health tools give clinicians not only trillions of genomic data points that they otherwise could not access but also millions of other data points that they otherwise would not have time to engage.
More importantly, wherever precision health tools help us understand why people are getting sick or what makes them more likely to get sick, public health practitioners can create and advocate for interventions that can keep people out of the doctor's office in the first place. That's good news for Alice and for everyone.
This article first appeared in the fall 2017 issue of Findings, the magazine of the University of Michigan School of Public Health.
- Learn more about precision health at the University of Michigan.
- Support precision health research at Michigan Public Health.
About the Author
Sharon Kardia is Senior Associate Dean for Administration, Millicent W. Higgins Collegiate Professor of Epidemiology, Director of the Public Health Genetics Program, and Director of the Life Sciences and Society Program. She received her master's degree in statistics and her doctoral degree in human genetics from the University of Michigan. She was then a post-doctoral fellow studying systems biology in the Department of Microbiology and Immunology. She joined the faculty of the University of Michigan School of Public Health in 1998. Dr. Kardia's main research interests are in the genetic epidemiology of common chronic diseases and their risk factors. Her research utilizes genomic, epigenomic, transcriptomic, and proteomic measures on large epidemiological cohorts.
